The combat environment exposes Service members to a great deal of complex sensory information and efficient performance relies on adequate function of the senses. Explosive blasts, however, can dramatically perturb the body's sensory system and have both short- and long-term health consequences. The auditory and vestibular systems, responsible for hearing and balance, are especially sensitive to blast, and deficits in these systems can alter the detection, identification, and localization of sound critical to the interaction of Service members with their environments.
In July of 2018, Carlos Esquivel and colleagues of the DoD Hearing Center of Excellence released an updated Joint Trauma System Clinical Practice Guideline (JTS CPG) titled "Aural Blast Injury/Acoustic Trauma and Hearing Loss" that officially superseded its 2016 predecessor. This CPG was then published in the September/October 2018 special issue of Military Medicine.1 The stated goal is to elevate the awareness of noise threat and to improve outcomes by encouraging early referral such that treatments can be initiated within the narrow therapeutic window .
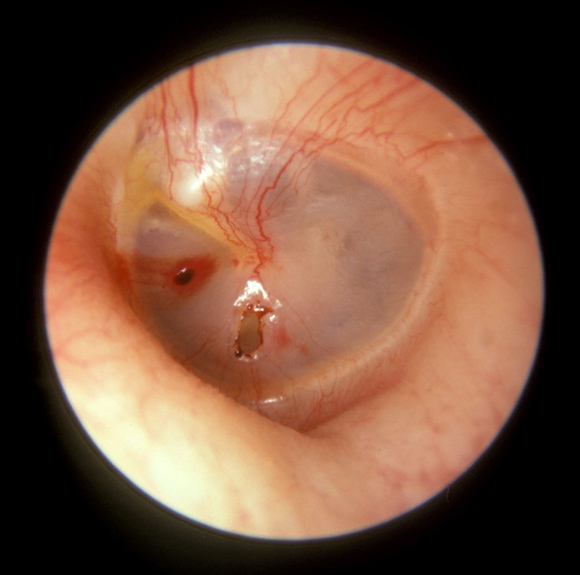
Noise levels above 140 dB can induce acoustic trauma with symptoms including hearing loss, tinnitus (ringing in the ears), ear pain, and vertigo (spinning sensation). Explosive blasts often surpass this noise threshold and can perforate the tympanic membrane (ear drum) and fracture or disarticulate the sensitive chain of inner ear bones; this is in addition to risks related to secondary and tertiary blast injuries including temporal bone fracture. Signs and symptoms of tympanic membrane rupture [see image] include symptoms of acoustic trauma as well as bloody discharge and conductive hearing loss (reduced ability to transmit sound from the middle to the inner ear). Dizziness or vertigo may be the results of traumatic brain injury, secondary infection, or other inner ear abnormalities.
The revised CPG recommends that medical providers should observe the following guidance: Service members who develop symptoms consistent with acoustic trauma should be asked about, or guided to self-report, acute tinnitus and hearing loss after life- and limb-saving procedures are complete. If debris is found in the external auditory canal or middle ear, fluoroquinolone and steroid containing topical antibiotics should be initiated; the debris should NOT be removed, and the ear should NEVER be irrigated as this may provoke pain, dizziness, and/or infection. Any patient reporting hearing loss or tinnitus should be referred for a hearing test.
Patients should be referred to otolaryngology (ENT) for:
Medical management adhering to this CPG can more readily return injured Service members to duty and possibly mitigate long-term hearing or balance deficits in Veterans.
Read the Joint Trauma System Clinical Practice Guideline (JTS CPG )
1 Esquivel CR, Parker M, Curtis K, et al. Aural Blast Injury/Acoustic Trauma and Hearing Loss. Military medicine. 2018;183(suppl_2):78-82.
Your 15 minute session will timeout in approximately 10 minutes.
If you're in the middle of entering information, please close this warning and save your progress (if possible) or finish up your task.
If your session fully times out, you will lose any un-saved work.
Your current Blast Injury Research Program session has expired.
Your next click will take you away from the private area, and you will lose any work you have in-progress.
Please enter your email address, and try again.